Actually, it is always allergy season in Texas. This month we are coming off the peak in Cedar Fever and growing into grass, ash, and oak. Thanks to our warm climate, things never really “die” in Central Texas so we can’t really lay claim to a single allergy season; it’s more about which allergen is high or low at a given time. As well, there is never a time we are not exposed to non-pollen things like animal dander, dust mites, mold, and even cockroaches.

We asked Dr. Candice Weiner, a primary care physician at St. David’s Georgetown Hospital for some basics about allergies and when it’s time to see the doctor.
The Basics
Typically, when our bodies have first contact with something perceived as harmful, we feel fine. Meanwhile, inside, we are making Immunoglobulin E (IgE) antibodies specific to fighting that substance if we are exposed again. “At the second exposure,” Dr. Weiner says, “the allergen finds those new antibodies and sets off a cascade of reactions. The antibodies seek out mast cells [mastocytes], which ‘explode’ with alot of histamines. Those histamines do a great job of fighting off the foreign agents, but they also do a good job of making you feel horrible. This is when you start sneezing, itching; your nasal passages fill with fluid and you get watery eyes, a rash, and more. So, histamines are great about fighting off those invaders, but your body is being overzealous because these allergens won’t really harm you.”
Some Facts
Allergies may also be present due to genetics; identical twins have the same allergies about 65 percent of the time. Children typically do not present allergies before they are about two years old, and they seem to peak between 8-9 years old and young adulthood. They often happen after a change in geography; when the body is exposed to many new elements at once; e.g., moving to Texas from a northern climate where pollen is covered with snow half the year.
Dr. Weiner says it is not known what causes allergies to come and go throughout our lives, “but we may be able to look forward to fewer reactions as we get older and immune responses become weaker in general.”
She adds that allergies also appear to be on the rise. “Where there are no conclusive data, some think modern life means more airborne pollutants, many that are microscopic and can more easily find their way to our mucous membranes. Some even postulate our improved hygiene and reduced exposure to dirt has helped cut down on disease, but prevented our exposure to so-called ‘good’ bacteria and other elements that used to train our immune systems.”
Is it a cold or the flu?
Dr. Weiner says there is overlap, but, “allergies may give you a scratchy throat, but without the horrible pain and swollen feeling. Cold and flu usually don’t last as long, so if you are the type to ‘tough it out’ but feel unwell for more than 10 days, it is likely not a virus.”
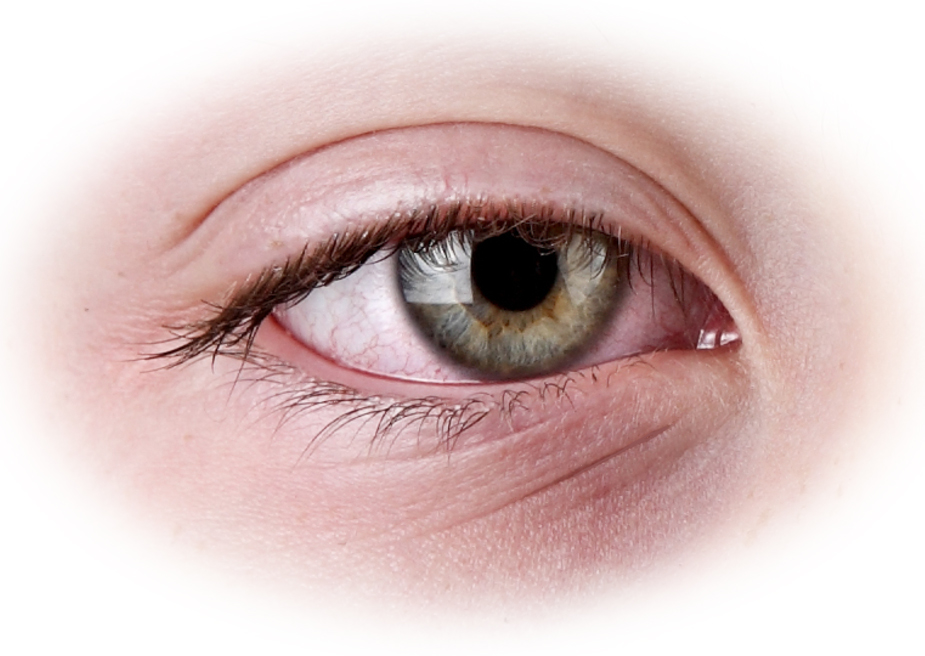
She also recommends being more cautious with children; i.e., not letting them be sick for several days without trying to determine the cause. Certain facial features can indicate an allergy spell. “An ‘allergic shiner’ is a swelling close to the eye, under the nose, usually with skin discoloration. Dennie-Morgan folds appear under the eyes; and possibly a horizontal crease at the top of the nose, caused by swiping an itchy nose up from fingertips to the base of the palm.”
Another distinction, she says, is that allergies come on quite quickly, whereas a cold or flu may have you feeling gradually worse over several days.
What to do
There are two tests to determine the thing(s) to avoid. A Patch Test “looks like a very large Band-aid, with many small allergen pockets. There is also a Prick Test, which exposes the skin via small needles with allergen tips. It looks scary, but I had it done myself and it’s not at all like getting a shot. Feels more like a back-scratch, so there is nothing to be afraid of and it’s very beneficial to know what your specific triggers are.”
A common solution is to have allergy shots, which introduce allergens to the body in very small doses. Shots are given, with decreasing frequency, until the antibodies learn that the substance is not lethal. “They are not a quick fix, but actually stop the allergy by blocking the pathway that created the reaction in the first place. It is also a preferred option if you want to avoid taking several pills or nasal doses every day.”
There are many over-the-counter medicines that can help alleviate symptoms, but she strongly recommends speaking with a doctor about side effects; “Just because it is OTC does not mean that it is not harmful. For example, Claritin-D has the same ingredients as Sudafed, which not only constricts blood vessels in your nose, but everywhere else too. So, if you have high blood pressure, it will make your nose stop running, but it is very bad for your circulatory health.” She also recommends keeping track of your response seasons and start your symptom treatment a week or two earlier each year to build up your non-response ahead of time.
Some of her patients recommend local honey as a natural option. There is no scientific evidence that it is a cure, but a teaspoon or two a day introduces microscopic allergens in a natural way, with no side effects. “Honey is also a natural antioxidant, thins out mucous, and can help with a cough.”
In any case, it is time to call the doctor if you have allergies, but also develop symptoms of flu or cold; one does not preclude having the other. “Doctors can not cure any of those three, but we can certainly help you feel a lot better.”
Considering the 2020 flu season is expected to last late into March, it’s good advice.
